People with HIV who started antiretroviral treatment early, before their CD4 T-cell count fell below 800, had a substantially smaller viral reservoir, according to study findings published in Clinical Infectious Diseases. Having a smaller reservoir of latently infected CD4 cells improves the prospects for long-term remission.
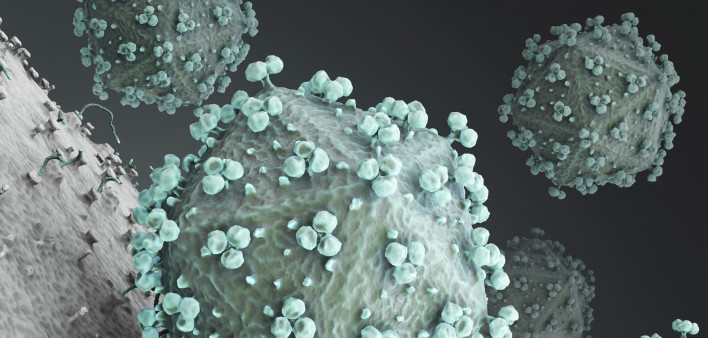
While antiretroviral therapy (ART) can keep HIV replication under control as long as treatment continues, the virus inserts its genetic blueprints into the chromosomes of human cells and establishes a long-lasting latent reservoir that is unreachable by antiretrovirals and usually invisible to the immune system. These so-called HIV proviruses can lie dormant in resting CD4 cells indefinitely in the presence of antiretrovirals, but they usually start churning out new virus soon after the drugs are discontinued. Prior research has shown that people who start treatment early have a smaller viral reservoir and may be more likely to achieve remission in cure studies.
Thomas Rasmussen, MD, PhD, of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne in Australia, and colleagues assessed the association between an individual’s CD4 count at the time of treatment initiation and HIV persistence while on ART.
The study included 149 people with HIV in Peru, South Africa and Uganda who participated in the Strategic Timing of Antiretroviral Treatment (START) trial. In 2015, this trial confirmed that starting treatment early leads to better outcomes than waiting until a person’s CD4 count falls below 350, which was previously used as a threshold for starting ART in an effort to reduce side effects. Today, guidelines recommend treatment initiation as soon as possible after HIV diagnosis.
The study participants were divided into three groups: those who started treatment with a CD4 count of 500 to 599 (36 people), 600 to 799 (60 people) or 800 or higher (50 people). Overall, the median age was about 40 years, 60% were women and more than 80% were Black, but those who started treatment with a higher CD4 count were older and were more likely to be women. Most participants used regimens containing nucleoside reverse transcriptase inhibitors plus a non-nucleoside reverse transcriptase inhibitor.
After three to your years on ART, the researchers measured levels of total HIV DNA, a specific type of HIV DNA (two-long terminal repeat HIV DNA) and cell-associated unspliced HIV RNA in CD4 cells. Plasma HIV RNA viral load was measured using a single-copy assay. They also measured expression of various cell surface markers on T cells, including HLA-DR, PD-1 and pSTAT5. These virological and immunological measures were compared across the three groups.
They found that total HIV DNA, plasma HIV RNA and HLA-DR expression (a measure of T-cell activation) were significantly lower in people who initiated treatment with a CD4 count of 800 or higher compared with the two groups that started ART later. Specifically, HIV DNA was 75% lower in those who started with 800 or more CD4 cells compared with those who started with 500 to 599 cells. Higher pSTAT5 expression significantly correlated with lower HIV DNA and HIV RNA levels in all groups. What’s more, these virological measures were significantly lower in women compared with men.
Initiating ART with a CD4 count of 800 or higher “was associated with achieving a substantially smaller HIV reservoir on ART,” the study authors concluded.
“Notably, HIV persistence on ART was greater in males than females,” they added, suggesting that “this may relate to the stronger innate and adaptive immune responses in adult females” and the potential role of estrogen, which suppresses HIV reactivation.
As a limitation of the study, the researchers acknowledged that because of the limited number of cells available for analysis, they were unable to analyze HIV-specific T-cell function, quantify the frequency of cells containing intact HIV proviruses or measure the frequency of cells with replication-competent virus. In addition, study participants did not start treatment with integrase inhibitor regimens, which are commonly used today.
“Taken together, these findings suggest that people with HIV who are able to preserve CD4 T cells ≥800 cells/mm3 before ART initiation, especially females, have a smaller reservoir on ART,” they wrote. “Interventional cure studies in this subgroup could potentially have a favorable outcome.”
Click here to read the study.
Click here for more news about HIV cure research.






1 Comment
1 Comment