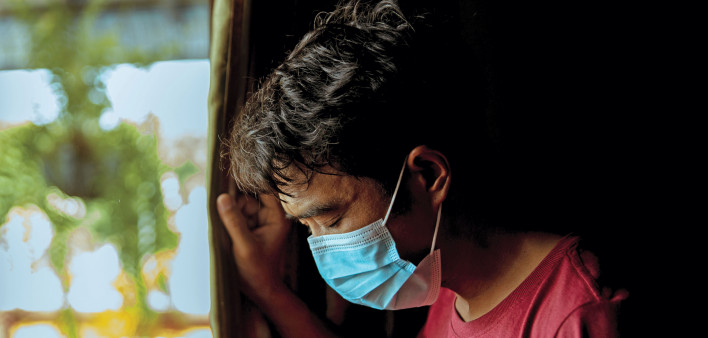
Long COVID, also known as post-acute sequelae of SARS-CoV-2 (PASC), refers to symptoms that last months or years after a bout of COVID-19. These may include shortness of breath, fatigue, brain fog and muscle and joint pain. The causes are not fully understood, but lingering organ damage, persistent SARS-CoV-2 infection and lasting immune system changes may play a role.
Michael Peluso, MD, of the University of California, San Francisco, and colleagues compared symptoms and measured SARS-CoV-2-specific immune responses in 39 HIV-positive people and 43 HIV--negative people recovering from COVID. They were diagnosed between April and December 2020 and had not yet received COVID vaccines. The HIV-positive participants were on antiretroviral therapy, most had an undetectable viral load and the median CD4 count was approximately 600.
Overall, people with HIV were about four times more likely to have long COVID. Some of the most common symptoms were at least twice as frequent in HIV-positive people compared with HIV-negative people, including fatigue (42% versus 23%) and concentration problems (42% versus 19%). Both groups had broadly similar antibody and T-cell responses, but people with HIV had lower levels of SARS-CoV-2-specific memory CD8 T cells and higher PD-1 expression, a marker of immune cell exhaustion, on SARS-CoV-2-specific CD4 T cells. People with HIV also had higher levels of certain inflammatory cytokines, which were associated with long-lasting symptoms. The researchers noted that long COVID may be driven in part by ongoing inflammation, and people with HIV are already prone to persistent immune activation and chronic inflammation.
“We observed that HIV status was strongly associated with PASC, raising concerns that this condition might be common among people with HIV recovering from COVID-19,” the authors wrote. “Larger and more detailed studies of PASC in people with HIV are urgently needed.”






Comments
Comments