When peer HIV testers explained the science behind Undetectable Equals Untransmittable (U=U), men were 89% more likely to agree to be tested for the virus, according to a pilot study published in AIDS and Behavior.
The U=U message, spearheaded by people living with HIV through the Prevention Access Campaign, translates the science of multiple randomized controlled trials of HIV transmission among straight and gay couples. Put simply, it explains that if you are on consistent HIV treatment for at least six months and have an undetectable viral load, not only will you live a longer, healthier life, but you will not transmit HIV to your sexual partners.
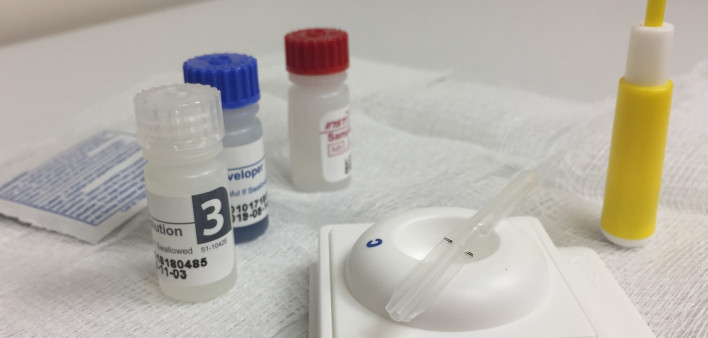
The trial launched in March 2020 and was meant to run for eight weeks—enough time to gather data from 4,000 men at five different mobile HIV testing sites around Cape Town in South Africa. In the study, 2,000 men were slated to receive the standard “Know Your Status” message and 2,000 were to be informed about U=U. However, 12 days into the trial, the COVID-19 pandemic led to a lockdown throughout the country, so the trial includes data from only 1,050 men.
The participants were a median of 35 years old and were well matched, with the exception that men in the U=U group were less likely to be employed.
Of those 1,050 men, 180 agreed to an HIV test. And of those, 112 men were randomized to the U=U group and 68 were assigned to receive the “Know Your Status” message. That comes out to 22% of the men in the U=U group getting tested for HIV, compared with 13% in the standard-of-care group.
That means that men randomized to the U=U group were both 61% more likely than their standard-of-care brothers to respond to the testing invitation and 89% more likely to stick around and actually receive an HIV test. In addition, 10 men received HIV diagnoses, seven in the U=U group.
However, that did not translate to linkage to care. Two men in each group were linked to care and offered HIV treatment within six weeks—but that means that four of the men in the U=U group weren’t successfully engaged in care. (One of the seven men in that group was already on treatment.)
Although these results are promising, Philip Smith, MSS, a socio-behavioral scientist at the Desmond Tutu HIV Centre and Foundation, and colleagues cautioned that the findings are preliminary. With only a quarter of the 4,000 invitations sent and 180 participants tested, the study had just enough power to determine that U=U messaging was associated with higher odds of testing. But the unexpected end of the trial because of COVID-19 means the researchers may have missed nuances in understanding the impact of the U=U message. Plus, they wrote, the same peer outreach workers sent out both the standard-of-care invitations and the U=U invitations, varying them by day. It’s possible that the messages weren’t consistent. But it’s still a hopeful sign for better testing and better outcomes.
“U=U messaging may work to assuage men’s fear of testing HIV positive and reassure them that an HIV diagnosis does not necessarily require them to alter their lifestyle,” Philips and colleagues wrote. “Even though men in the U=U study group were more likely to return for an HIV test, there was limited difference between the two groups on U=U knowledge. This may suggest a selection effect in which the U=U message motivates testing without the participants having to cognitively engage with or recall the specifics of messages.”
Click here to read the full study.
Click here for more news about U=U and news about HIV testing.






1 Comment
1 Comment